An overview of IVF treatment for Infertility
I would like to give you an idea of what happens during an In Vitro Fertilisation (IVF) treatment to help demystify the process and explain why we do what we do.
What is the female body doing normally to reproduce?
In most women, each month, a batch of eggs is maturing towards ovulation. Soon after a period starts, the egg that is developmentally slightly ahead of the rest (ahead because it “started the race earlier”, not because it will be the “best”) is allowed to continue developing and the rest of the eggs in that batch die off. Once that egg reaches maturity a hormone (LH) is released “triggering” the egg to ovulate. (If you are trying to conceive) hopefully the egg meets a sperm in the fallopian tube, fertilises, develops for about five days while travelling down the tube and into the uterus and, on day five or six after fertilisation, implants into the lining of the uterus. Meanwhile the ovary has continued to produce hormones (mainly progesterone) to keep the uterus quiet and ready to receive the embryo.
IVF treatment involves manipulating hormones to help your body produce more eggs.
In an IVF cycle the same hormone your body usually uses to make eggs mature (FSH) is given but at a higher dose than your body would usually produce – so more of the batch of eggs matures rather than just the one. That is you will grow the egg that was going to mature and ovulate anyway and some of the ones that would have otherwise have died off, not eggs for future cycles.
The medications will only work on eggs that have “started the race”, we will have an idea of this number through ovarian reserve tests undertaken prior to starting IVF. IVF treatment does not use up your reserve eggs.
A second medication is then given to prevent your body signaling for those eggs to ovulate (ie. To prevent you “triggering” ovulation) and allow us to time your egg retrieval.
I “watch” your ovaries with blood tests and ultrasounds to judge when your eggs are mature (usually two or three blood tests +/- ultrasounds over about 10 days) and, when I judge your eggs are mature, you give yourself a medication that works like LH and signals to the eggs to get ready to ovulate. This is the “trigger” medication.
This medication is timed precisely.
The medications (FSH, LH, trigger) are all injections. The needles are very small and need to be inserted just under the skin. Most women who do IVF have never previously given themselves an injection – the injections are designed to be simple to use and you will be shown how to give them. Some women prefer their partner or a friend to give the injections, some prefer to come to the clinic for a nurse to give the injection. Most women find the injections much easier than they expect.
Oocyte Pickup: How we retrieve the eggs.
Just before ovulation the eggs are removed from your body. The egg retrieval is usually undertaken with a light anaesthetic. A vaginal ultrasound probe is placed against each ovary and, under the guidance of ultrasound, a tiny tube is placed into each ovary and the follicles (the fluid filled sacs where the eggs are growing) are emptied.
What happens once the eggs are retrieved?
The fluid from the follicles is passed over to a scientist (embryologist) to examine and identify your eggs.
Once your egg retrieval is complete we need sperm. Depending on the circumstances a fresh or frozen sample is used.
The sperm and eggs are then brought together – simplistically this is either 50,000 or so sperm put in a dish with each egg and left to their own devices or ICSI, where a single sperm is injected into each egg. In some circumstances it may be of benefit to use specialised methods to select which sperm to use (PICSI, IMSI).

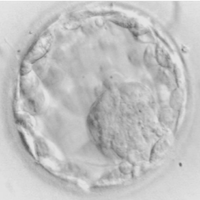
Your eggs and sperm are then nurtured in a highly specialised culture fluid inside an incubator overnight and checked the next morning for signs of fertilisation. Your fertilised embryos will be grown, usually for five days and the embryo that looks the strongest placed into your uterus five days after the egg retrieval. This procedure feels similar to a pap smear. An ultrasound probe placed on your lower abdomen will let you see the fine catheter (tube) being threaded through your cervix into your uterus (most women do not feel this). The embryo is gently flushed out of the fine catheter and into your uterus.
Any remaining embryos judged of good quality are cryostored (frozen) – ideally for a second or third baby later, but if the fresh embryo does not result in an ongoing pregnancy a frozen embryo can be transferred the following month.
After the embryo is transferred another support hormone will be given to keep your uterus quiet – giving the embryo a chance to implant.
And the wait for a much anticipated pregnancy test begins.
Treating Infertility: What I offer you as a Fertility Specialist.
There are numerous ways to run an IVF cycle. In some circumstances there will be benefits to different protocols – whether that be the medications used to mature your eggs, the medications used to suppress your own ovulation, the trigger medication, the post ovulation (luteal) support medication or other additional medication or laboratory procedures. We will talk through these options and my recommendations when planning your cycle and during the cycle as I see how your body is responding.
More information about IVF cycles can also be found on the Monash IVF website.
Information on why I choose to work with Monash IVF can be found here.



